Medical Journal of Australia, Volume 1: Pages 1083-1086, 27 May 1967.
Royal Newcastle Hospital, Newcastle, N.S.W.
IN 1949 Gairdner drew attention to the fact that circumcision is one of the commonest operations performed, yet it is accorded the least critical consideration.
In our community, circumcision of the newborn male is frequently requested or demanded as a right by the parents, and just as often is performed after a minimum of medical thought as to the need for it, or its effects.
In the writer's view, the design and behaviour of the prepuce is as skillfully adapted to the needs of the newborn infant male as any other part of his anatomy. Removal of it may be to his detriment.
The prepuce has an essentially protective role. It is no accident that the prepuce is not normally retractible until the age of three, four or five years. By this time the child no longer wears napkins, and the danger of injury from friction or chemical or bacterial irritants is much less.
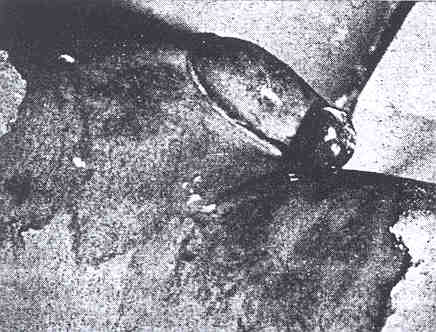
Figure 1 illustrates an example of the protective function of the foreskin. This boy had suffered second degree burns to the pubis, thighs and genitalia. The prepuce was involved and swelled considerably, but throughout the boy's treatment and convalescence he voided normally, with no evidence of dysuria. Had he been circumcised, the glans would almost certainly have suffered injury with subsequent scarring, and meatal stenosis might well have resulted.
The development of the prepuce is not complete at birth, and at this time the foreskin is rarely retractible. This non-retractibility must not be taken as an indication for circumcision. In fact, it is hard to imagine a medical indication for circumcision at this age. By simple but incomplete withdrawal of the prepuce it can nearly always be demonstrated that the meatal opening is larger than the urinary meatus.
Phimosis
True phimosis is not common. Hospital reports are confused, as the term is used loosely to justify social
circumcision, and description of the actual pathological finding is often conspicuous by its absence. To diagnose phimosis, one must find not only a non-retractile foreskin, but a small preputial opening. Ballooning
of the prepuce occurs on micturition.
Paraphimosis
Paraphimosis, too, is rare in young children. It is doubtful if one episode constitutes an indication for circumcision. Rater does it emphasize the necessity for education of the parents. Clinic sisters often advise mothers of uncircumcised boys to retract the prepuce during bathing. It has already been pointed out that this is unphysiological under the age of three to five years, and should be discouraged. When the prepuce is freely retractable it is legitimate and perhaps advisable to retract it in the bath provided that the parent ensure that it is reduced again to its previous state. Surgery is no substitute for education of the public in normal anatomy and physiology.
Chronic or Recurrent Balanoposthitis
Recurrent infection under a non-retractable foreskin in an older child (it is rarely seen in the infant) seems a more legitimate reason for recommending operation to allow drainage. In the acute stage, if operation is necessary after failed conservative measures, the performance of a preliminary dorsal slit may be a safer procedure. The fortunate rarity of this condition in infants is possibly the result of the persisting attachment of the prepuce to the glans. It occurs more commonly in elderly diabetics.
Posthitis-a Contraindication
Inflammation of the prepuce, often participating in a generalized skin infection of the nappy area, is occasionally cited as an indication for circumcision. The writer is emphatic that it is an absolute contraindication to the operation, as it exposes the glans and meatus to the same pathological process. Other contraindications such as hæmophilia and hypospadias are well known.
No method of circumcision is perfect. In adults and older children, the standard cut, ligature and suture method is most commonly used and is quite satisfactory. For neonates, many quicker methods have been devised. The bone forceps technique is effective, yet occasionally the glans and urinary meatus are damaged, with disastrous consequences. Personal experiences with the clamp method (Gumco
or Little Trimmer
) have been unsatisfactory. These clamps are designed to offset the danger of the bone forceps while still retaining the advantage of speed. In a significant proportion of cases hæmostasis is incomplete, and recourse must be had to ligature and suture.
The newer Plastibell
technique, originally designed for circumcising the baby at birth, has much to recommend it (as a method) for the neonate. It is quick and relatively safe compared with other methods. The prepuce is separated from the glans after a small preliminary dorsal slit has been made, and the Plastibell
is inserted over the glans under the prepuce, which is then tied with tightly round it at the base with a thread. The prepuce beyond the thread is then excised, and the Plastibell
remaining in situ as a hæmostatic agent. The baby may be bathed normally (and should be to keep the penis and attached foreign body clean), and the bell
and thread fall off on the fifth or sixth post-operative day. There is a foreign body reaction with mild redness and swelling, but the ultimate result is good. The advantages are speed, relative safety from bleeding (see below), no bathing restrictions and a good result.
The immediate complications are bleeding, infection and damage to the glans. Death can result from the first two, or indirectly from anaesthesia. The remote complications are those which result from the removal of the nature-given protective action of the prepuce, namely, meatal ulcer and stenosis.
Death is fortunately rare, yet it does occur. In Australia there was a death in 1963 and one in 1964 from circumcision (Table 1). In England and Wales, from 1960 till 1964 inclusive, there were six such deaths of infants and children.
Bleeding is occasionally a source of worry, and anyone confronted with it cannot help regretting that he agreed to circumcise the child because the parents demanded it.
Infection in rare. The wound always looks superficially infected, but clinical evidence of bacterial invasion is not often seen.
From March, 1963, till January, 1966, the writer performed, or was responsible for the performance of 822 circumcisions of infants and children. The records of those have been reviewed, and those of all patients admitted to the Royal Newcastle Hospital, during the same period of time, suffering from complications of circumcision or the consequences of not being circumcised, werealso studied.
Details of the 822 circumcisions are shown in Table 2. Seven hundred and eighty-eight of these were non-therapeutic neonatal circumcisions. Twenty-one were non-therapeutic procedures in older children and only 13 were medically indicated.
Neonatal Circumcisions
Neonatal circumcisions were all performed or attempted with the use of the Plastibell
technique. Three types of early complications were seen. The immediate one was bleeding at the time of the operation. This may be the result of the following occurrences.
It was found that the only way to control such bleeding was to remove the Plastibell
and resort to the ligature andsuture method.
Retained Plastibell
was the commonest complication. Instead of falling off the fifth or sixth day, the rim was still in situ when the baby was brought back for review after a week. Removal was quite easy and posed no problems.
Infection as such was not seen. A foreign-body reaction was often mistaken for infection by resident medical officers, but always settled on removal of the Plastibell.
From March, 1964, till January, 1966, accurate records of these complications were kept as a prospective study. The incidence of primary bleeding was 2% (8 cases) and of retained Plastibell
11% (41 cases).
Non-Therapeutic Circumcision of Older Infants and Children
Twenty-one boys were circumcised by the cut, ligature and suture technique under general anæsthesia. These circumcisions were all carried out because of parental demand. Attempts were made to persuade such parents of infants beyond the neonatal period to wait till they were aged one year before having the operation done. When the infants are aged over six to eight weeks general anæsthesia is necessary. There were no serious immediate complications in this group. (It must be emphasized that the views expressed above, based on this series and previous experience, have caused this writer to discontinue the policy of consenting to perform circumcisions on parental demand only, without a medical indication.
Therapeutic Circumcision
Details of the 13 boys circumcised for medical reasons are given in Table 3. Five circumcisions were performed for true phimosis. It may well be argued that if it had not been for the large number of prophylactic operations the number of therapeutic procedures needed would have multiplied many times. Yet it is hard to believe that it wouldhave approached 700.
Meatal stenosis is the all-important late complication of circumcision. During the period under review (March 1963, till January, 1966), 28 boys were seen at the Royal Newcastle Hospital by the writer and other surgeons with meatal stenosis sufficiently severe to require meatotomy. Four others were admitted to hospital because of meatal ulceration which did notprogress to stenosis.
Meatotomy is a simple procedure, but it does require a general anæsthetic. The children presented with dyuria (screaming on mictirition) because of ulceration and crusting over the meatus, frequency of micturition caused by the tiny opening or, in one case enuresis. All were cured by meatotomy. Their ages varied from one to nine years. It must be emphasized that these 28 cases were not drawn entirely from the series discussed above. The occurrence of the condition is not related to the method of circumcision or the skill with which it is performed., for it is a late complication. It is simply the consequence of the loss of protective foreskin.
This common complication of circumcision, requiring further surgery, provides one of the strongest arguments against routine removal of the prepuce. It is certainly indicates the fallacy of the argument that boys should be circumcised so they will have no trouble in laterlife.
To present both sides of the picture, one must refer to other patients who required admission to hospital, during the same period, because of bona-fide complications of still being in possession of a foreskin. The following remarks apply to all patient admitted to the Royal Newcastle Hospital between March, 1963, and January, 1966, and not only to the writer'scases.
Paraphimosis
There were seven patients admitted to hospital with paraphimosis during this period. Their ages ranged from four to 47 years; three were children, two adolescents and two adults. Two were treated by simple reduction of the prepuce; the others needed reduction of the prepuce and circumcision.
Phimosis
Five of the writer's cases of phimosis have been mentioned above. In addition there were several children with phimosis who were circumcised by other surgeons, and 11 adults who were similarly treated.
Balanoposthitis
There were six adults with recurrent or chronic balanoposthitis who required circumcision. Four of these were diabetics.
![]() Note:
Note:
There is not doubt that early circumcision prevents the development of carcinoma of the penis. The carcinogenic properties of smegma are implicated as the causal agent. Sampson Handley (1936) advocated routine preputiotomy
(the making of a dorsal slit) for neonatal boys as a prophylaxis against this neoplasm. Were carcinoma of the penis as common as lung cancer, preputiotomy or routine circumcision would be justified to prevent it. Table 1 gives the death rate in Australia (1960 to 1964 inclusive) from penile cancer and non-therapeutic circumcision.
During the period March, 1963, till January, 1965, only three patients were admitted to the Royal Newcastle Hospital with penile carcinoma, and only one of these wasa new case.
If circumcision were entirely without complication and disadvantages, its use as a prophylactic measure would be justified, even with a low incidence of penile cancer. Yet it is not. Nor is it clear whether carcinoma of the penis is prevented by adequate personal hygiene in the uncircumcised. This may well be a safer means of prophylaxis.
Sampson Handley (1936) drew attention to a possible link between the incidence of carcinoma of the uterine cervix and the incidence of circumcision in the male sexual partners. He pointed out that Jewesses infrequently suffer from the condition. In Fiji, fewer cases of carcinoma were seen among Fijian women than among immigrant Indian women. Fijian males are circumcised at puberty, while Indian males remain uncircumcised. Many subsequent papers have written on the subject, but the evidence is slender. Wynder et alii (1964) conducted a controlled study, and found that between five and eight per cent of the white non-Jewish cervical cancer population were effectively exposed only to circumcised males, while the comparable figure for the controls were between 14 and 18 per centum.
Janes et alii (1958) however, in an extensive study of the epidemiological factors involved in carcinoma of the cervix, also matched control subjects and cancer patients, and concluded that circumcision, or lack of circumcision, was as frequent in partners of cases with cancer as in cases of controls.
There seems little doubt that human smegma is carcinogenic (Heins et alii, 1958; Pratt-Thomas et alii, 1956). If indeed, it is true that the wife of an uncircumcised male is subject to a slightly greater risk of developing cervical carcinoma because of smegma under the prepuce, it may be that adequate male hygiene would protect her as much as circumcision of her husband. Carcinoma of the cervix is more common amongst the poorer classes (Jones et alii, 1958), and it is reasonable to assume that their standard of personal hygiene may be lower than that of others morefortunate.
Though the risks of circumcision are not great, they must be weighed against the very dubious benefits. The procedure is performed as a social custom rather than a form of medical prophylaxis. So real are the disadvantages ensuing from loss of the foreskin that the writer is firmly of the opinion that non-therapeutic circumcision should no longer be performed.
Certainly, these views have been expressed many times, yet the normal anatomy, physiology and protective function of the foreskin are still understood poorly by recent medical graduates, and by the public not at all. Accordingly, this paper has been written in the hope of stimulating a continuing interest in the subject. If some thought and argument is provoked, however little in agreement with the writer's views, the paper will have achieved its purpose.
The foreskin has a definite purpose—protection of the urinary meatus and the incompletely developed glans penis. A non-retractable foreskin in the neonate and infant is normal, for the process of separation from the glans is incomplete at birth.
The untoward consequences of the operation are those resulting from the loss of protective functions of the foreskin-meatal ulceration and stenosis. The operation itself has a slight but very real danger.
Circumcision is effective in preventing phimosis, paraphimosis and penile carcinoma, but the view is expressed that the balance of risks argues against the practice of non-therapeutic circumcision as a routine prophylactic measure. The ultimate decision must be based on more adequate evidence of the incidence of complications of being uncircumcised; it is a decision to be made by the medical profession rather than by the dictates of social demand.
The Fate of the Foreskin, A Study of Circumcision,Brit. med J.,2 : 1433.
The Prevention of Cancer,Lancet, 1 : 987.
A Study of Epidemiological Factors in Carcinoma of the Uterine Cervix,Amer. J. Obstet. Gynec., 76 : 1.
The Carcinogenic Effect of Human Smegma. An Experimental Study,Cancer, 9 : 671.
A Study of the Environmental Factors in Carcinoma of the Cervix,Amer.J. Obstet. Gynec., 68 :1016.
The Circumcision Information and Resource Pages are a not-for-profit educational resource and library. IntactiWiki hosts this website but is not responsible for the content of this site. CIRP makes documents available without charge, for informational purposes only. The contents of this site are not intended to replace the professional medical or legal advice of a licensed practitioner.
© CIRP.org 1996-2024 | Filetree | Please visit our sponsor and host:
IntactiWiki.