Journal of Clinical Forensic Medicine, Volume 7: Pages 32-34, 2000.
1The National Centre of Forensic Medicine, 67 Ben Zvi Rd., P O Box 49015, Tel Aviv 61490, Israel. 2Department of Pathology, Chaim Sheba Medical Center and Sackler Faculty of Medicine, Tel Aviv University, Ramat Aviv, Israel. 3Division of Identification and Forensic Science, Israel Police.
SUMMARY. Lethal complications following ritual circumcision are extremely rare, the most common being sepsis. We present here a case of fatal haemorrhage from a tiny incision of the glans, following a "home" circumcision of a 6-week-old baby. The post-mortem examination disclosed idiopathic neonatal hepatitis. It is suggested that the previously undiagnosed hepatic condition was responsible for the fatal haemorrhage.
© APS/Harcourt Publishers Ltd 2000
Journal of Clinical Forensic Medicine (2000) 7, 32–34
Male circumcision is a simple surgical procedure performed all over the world, in the USA it is the most common operation performed in males.1 It is estimated that 1.2 million newborn males are circumcised in the USA annually. A great number of cultures including Jewish, Muslim, African, Australian, Polynesian and some South American aborigines practice male circumcision as part of their ritual traditions.2 About one in six boys and men in the world has been circumcised.2 The main potential medical benefits that support this practice include prevention of phimosis, paraphimosis, balanitis, a decrease in the risk of cancer of the penis and a reduction of the risk of urinary-tract infections among infants. The most common complications of circumcision include haemorrhage, sepsis and surgical trauma. It is estimated that the overall complication rate of this procedure ranges from 0.2 to 5%.4
Currently, there is an ongoing debate regarding the health advantages of circumcision. Although the American Academy of Pediatrics (AAP) stated in 1989 that there are no valid medical indications for circumcision in the neonatal period, their current position acknowledges that there are potential medi-cal benefits which must be weighted against its risks.5,6 There are very few reports in the literature regarding a lethal outcome from circumcision complications, most are from sepsis;7,8 500 000 consecutive circumcisions in New York were fatality free.1 We present the only case as far as we are aware, reported in the medical literature, of fatal haemorrhage due to a surgical misadventure in the course of a circumcision, in a baby affected by idiopathic neonatal hepatitis – a heterogeneous hepato-biliary disorder of undetermined cause.9
A healthy "small for date," 6-weeks-old male infant of Ethiopian origin, underwent ritual circumcision. The procedure was performed by his own father at home following the tradition of Ethiopian Jews.
The preputial skin was incised with a sharp and clean razor after being pulled over the glans and the inner preputial epithelium was freed with a rudimental metallic clamp. Profuse external haemorrhage from the surgery site developed almost immediately. The attempts to control the bleeding by applying continuous local pressure failed and 12 h later the infant was rushed to the nearby regional medical center. On admission the patient presented with severe hypo-volemia with an haemoglobin count of 6.6 g/%, severe metabolic acidosis and extreme bradycardia.
The baby was responsive only to painful stimuli, rectal temperature was 35.2°C and there was no further active bleeding from the glans, which was immediately covered with a thick film of gelatin foam (Gelfoam).
Despite immediate tracheal intubation with assisted respiration and administration of bicarbonate, adrenalin and atropine and fluids, the severe bradycardia persisted and he was pronounced dead 3 1/2 h later.
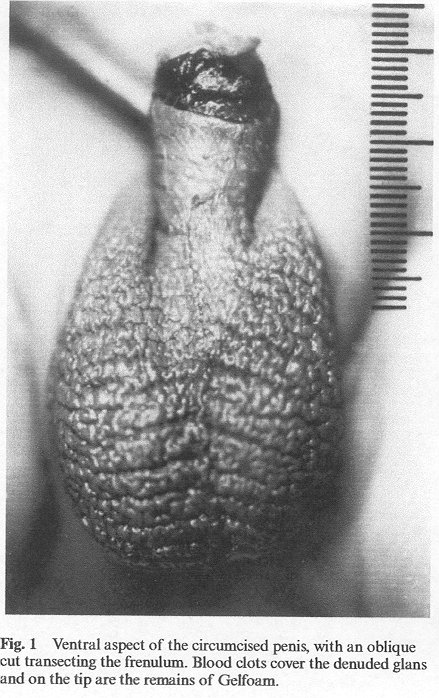
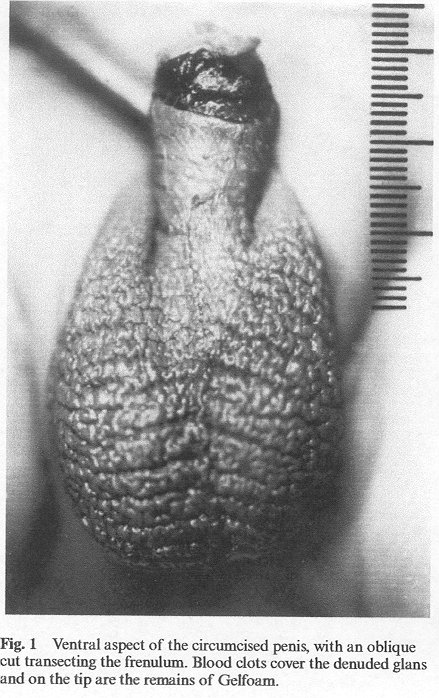
The following day an autopsy was performed at the National Centre of Forensic Medicine. The body weighed 2660 g, the crown-heel length was 51 cm and the head circumference was 32 cm. The conjunctivae were pale, with no petechial haemorrhages or yellowish discoloration. No external malformations or injuries were noted except for a small wound on the penile shaft covered by clotted blood and gelatin foam.
The total length of the penis was 2.2 cm, the whole prepuce had been removed through a horizontal incision on the dorsal aspect and an oblique incision towards the scrotum on the ventral side. The oblique cut transected the frenulum and incised the glans immediately above at the level of the corona glandis. No major blood vessel, such as the superficial dorsal penile arteries and vein, was cut. On the ventral surface the remaining skin covered 1.6 cm of the shaft while on the dorsal side 1.9 cm were covered. On the ventral aspect of the denuded shaft a 0.4 cm nick was detected, covered by small blood clots adhered to the wound (Fig. 1). Anatomical dissection of the penis did not reveal any structural abnormalities. Gross examination of the internal organs did not reveal abnormalities except for a micronodular appearance of the liver, which weighted 95 g (normal). Histological examination of all organs did not reveal abnormalities except for the liver, which showed various features of neonatal hepatitis, including severe lobular disarray with moderated mononuclear infiltration, macrovesicular steatosis, bridging fibrosis and areas of nodular regeneration. Scattered multinucleated giant cells, hepatocelular and canalicular cholestasis, excessive extramedullary haematopoiesis and moderated haemosiderosis were also observed (Fig. 2).
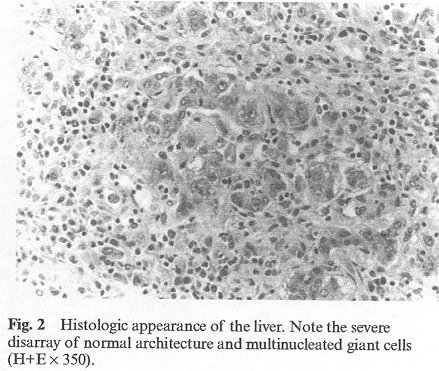
The cause of death was determined as severe hypovolaemic shock from a deep cut through the glans during circumcision. The profuse bleeding resulted from idiopathic neonatal hepatitis, which was diagnosed on the basis of hepatic microscopic examination only since serum tests for clotting disorders were not performed at the hospital.
In the Jewish tradition, circumcision should take place on the eighth day after birth and should be performed by a "Mohel" (a man, not necessarily a physician, especially trained for this religious task).10 Some congregations deviate from these ritual prescriptions and have the ceremony performed on a later date and by the male head of the family.11
The aim of circumcision is to excise sufficient fore-skin to leave the glans uncovered.12 The key factors to be observed are attention to asepsis, not excessive excision, haemostasis and cosmesis.13
In the majority of cases there is only minor bleeding from the incision, all that is required to achieve haemostasis is gentle pressure on the area. Complications arise as a result of the operator's inexperience rather than of the method employed.14 Excessive bleeding may be due to anomalous vessels 13 or the presence of a bleeding disorder.11
Although there are references to fatal complications of neonatal circumcision,15-17 the authors were unable to trace specific case reports in the medical literature. To the best of our knowledge, all fatal cases resulted either from complications of anaesthesia or sepsis.18 There are, however, cases of near-fatal haemorrhage following circumcision.
In the reported case the father of the infant, lacking the necessary experience, carried out the ritual procedure. The minuscule incision on the penile shaft, which on an otherwise healthy infant, most probably would have resulted only in minor bleeding, caused massive haemorrhage, in this infant who suffered from idiopathic neonatal hepatitis. The baby's death was the result of fatal bleeding, not only because of the delay in medical assistance – which cannot be underestimated – but mainly because of the underlying blood coagulation disorder. The severity of bleeding appeared to be related to the degree of liver-function impairment. The existing condition, which among others precipitates hypoprotrobinemia,19 was such that in this case the normal coagulation cascade was severely compromised.20
The circumcision debate is entering a new era. In 1989, the AAP balanced its stands concluding that "newborn circumcision has potential benefits and advantages as well as disadvantages and risks," their current position acknowledges that there are potential medical benefits which must be weighted against its risks.5,6
There are contraindications to newborn circumcision; patients with hypospadias, epispadias and megalourethra should not undergo circumcision at birth because the foreskin may subsequently be required for urethral reconstruction. Circumcision is relatively contraindicated on patients with bleeding diathesis, prematurity, and severe medical problems.4
The present case report should raise the awareness of the practitioner to the possible lethal complications resulting from a mishap during circumcision on a compromised child. Furthermore family physicians, neonatologists, obstetricians and paramedical staff, who are in contact with parents who desire to have their newborn circumcised, should advise them to request an expert and in case of any complications to report to a medical practitioner. This is the first reported case of fatal haemorrhage following ritual circumcision. A greater awareness of possible complications to this common and widely believed "safe," surgical procedure is suggested.
Correspondence to: T. Kahana, fax: 972-3-6833813; Tel.: 972-3- 5127857; e-mail: abctzipi@matat.health.gov.il
The Circumcision Information and Resource Pages are a not-for-profit educational resource and library. IntactiWiki hosts this website but is not responsible for the content of this site. CIRP makes documents available without charge, for informational purposes only. The contents of this site are not intended to replace the professional medical or legal advice of a licensed practitioner.
© CIRP.org 1996-2024 | Please visit our sponsor and host: IntactiWiki.