British Journal of Urology, Volume 83, Issue Suppl. 1, Pages 34-44. January 1999.
Departments of Pathology, Marshfield Clinic, Wisconsin, USA, and *
Health Sciences Centre, University of Manitoba, Canada
British Journal of Urology, Volume 83, Issue Suppl. 1, Pages 34-44. January 1999.
Departments of Pathology, Marshfield Clinic, Wisconsin, USA, and *
Health Sciences Centre, University of Manitoba, Canada
Keywords: Prepuce, embryology, development, anatomy, function, circumcision, histology
The prepuce is a common anatomical structure of the male1 and female2 external genitalia of all human and non-human primates; it has been present in primates for at least 65 million years, and is likely to be over 100 million years old, based on its commonality as an anatomical feature in mammals3 Certain cultures have excised the prepuce from children to conform to societal standards, while other cultures accept the complete external genitalia as normal (Fig. 1). The motives for circumcision in preliterate cultures are difficult to define, but include rites of passage, blood sacrifices and cultural markings4. Ritualistic, childhood genital surgery has become popular in the last several thousand years, making the prepuce the most vilified normal anatomical structure of the human body. Rather than acknowledging the prepuce as normal anatomy, some contemporary physicians consider the penile5 and clitoral prepuce (or clitoral hood)6,7 to be dangerous and unhealthy. However, before theoretical justifications for circumcision can be considered, a complete understanding of the normal anatomy and function of the prepuce is required. This paper reviews the embryology, anatomy and function of the prepuce.

The prepuce is an integral, normal part of the external genitalia that forms the anatomical covering of the glans penis and clitoris. The outer epithelium has the protective function of internalising the glans (clitoris and penis), urethral meatus (in the male) and the inner preputial epithelium, thus decreasing external irritation or contamination. The prepuce is a specialized, junctional mucocutaneous tissue which marks the boundary between mucosa and skin; it is similar to the eyelids, labia minora, anus and lips. The male prepuce also provides adequate mucosa and skin to cover the entire penis during erection. The unique innervation of the prepuce establishes its function as an erogenous tissue8.
Ritualistic circumcision involves the involuntary removal of normal, healthy genital tissue from infants and children for religious, societal or theoretical medical benefits. Although the amount of genital tissue removed is variable, the penile prepuce is removed in nearly all male circumcisions, and the clitoral prepuce is removed in a Fourcroy grade 1 female circumcision9 (see Elchalal, pp.103-108).
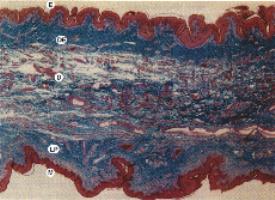
The male prepuce is formed by a midline collision of ectoderm, neuroectoderm and mesenchyme, resulting in a pentalaminar structure composed of a squamous mucosal epithelium lamina propria (corion) dartos muscle, dermis and outer glabrous skin10.
The embryology of the penile prepuce has been controversial since the original account given by Schweigger-Seidel in 186611, who described a preputial fold that progressively extended and fused with the epithelial covering of the glans. Glenister cited Retterer (1885-1915) as the first to show that the prepuce was formed by a combination of preputial folding and the ingrowth of a cellular lamella12. This ingrowth creates the prepuce, glans, corona and coronal sulcus mucosa. This results in a common mucosal epithelium of the glans penis and the inner mucosal lining of the prepuce. The squamous mucosa of the glans penis, coronal sulcus and prepuce should be considered as one tissue compartment10 with a common cytokeratin polypeptide pattern13.
20 22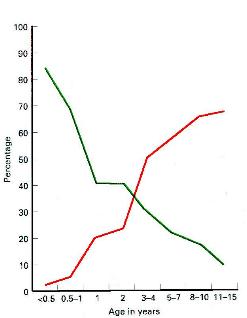
The fused mucosa of the glans penis and the inner lining of the prepuce separates gradually over years, as a spontaneous biological process. Topical steroid14-16 and nonsteroidal17 anti-inflammatory ointments are known to accelerate the glans-prepuce separation. In male rhesus monkeys exposed to intrauterine diethylstilbestrol, the normal separation of the glans/prepuce is delayed from a normal age of 2.5-3 years to 4.5-5.5 years18. Despite this research, the hormones and/or growth factors responsible for this separation of the glans-prepuce are poorly understood. Gairdner found that 96% of newborn males have a fused mucosa; in 20% of boys aged 5-13 years, he reported that the prepuce could not be completely retracted19. Øster confirmed in a large study that preputial non-separation (adhesions) is very common in children and teenagers. The separation of the prepuce/glans penis mucosa is usually complete by about age 17 years, as confirmed by later Chinese studies (Fig. 2)20,21. Recent work by Kayaba et al. verified that the preputial orifice may be tight in young boys, but resolves over time (Fig. 3)22. Without knowledge of the normal development of the penis, some physicians advocate childhood circumcision as a surgical treatment of normal anatomy5. One study stated that microscopic examination of the prepuce circumcised for phimosis showed normal histology in 46% of cases23. As the mean age in that study group was 8.7 years, almost half of these boys were circumcised for a normal stage of penile development22; a tight preputial orifice with normal histology is not pathological in young boys, but should be considered a normal stage of penile development. Neonatal circumcision, before the prepuce has naturally separated, involves tearing the common prepuce/glans penis mucosa apart, with the concomitant risk of glanular excoriation and injury. Manipulation and retraction of the immature prepuce must be avoided to prevent scarring, bleeding, phimosis and psychological trauma24.
Frequently after circumcision, the immature mucosa of the glans and the preputial remnant will fuse25. Of historical interest, true aposthia (absence of a prepuce) with normal development of the urethra and glans must be very rare: however, it is referenced in Jewish law of 1567 CE, relative to a child born circumcised26. This probably represented hypospadias with incomplete development of the prepuce. However, some authors believed that `aposthia' in Jewish males proved the effects of circumcision could be passed on in a Lamarckian-type hereditary transfer of somatic alterations26. Although it is generally accepted that normal preputial development is required for the successful canalization of the glans urethra27, hypospadias28 and epispadias29 have been reported with normal preputial development. These reports underscore the complex development of the prepuce and distal urethra. Megameatus with an intact prepuce30 and subcoronal hypospadias with complete prepuce31 are two other variants of hypospadias that are important to recognize as contraindications to newborncircumcision.
The clitoral prepuce develops similarly to that in the male12. The prepuce of the clitoris forms independently of the urogenital and labioscrotal folds, which form the labia minora and labia majora, respectively32. The clitoral prepuce is formed by a cellular lamella which grows down on the dorsum of the clitoris12 and is fused to the clitoris in the fetus33.
Some authors state that the clitoral prepuce is formed by a splitting of the urogenital folds around the clitoris, with development of the prepuce superiorly and the clitoral frenulum inferiorly34. However, this theory is discordant with earlier studies12 and has not been explicitly proved. The urogenital groove on the ventral surface of the clitoris prevents circumferential preputial development and results in the hoodlike appearance of the clitoral prepuce. The urogenital groove of the clitoris eventually regresses and develops into the labia minora32. In the female, there is no mesenchymal proliferation in the prepuce to form a dartos muscle layer. Physicians can allay parental fear of normal, intact external genitalia by explaining normal development and maturation. With this understanding, physicians will also be less likely to amputate normal, healthy genital tissue from children.
The male prepuce has somatosensory innervation by the dorsal nerve of the penis and branches of the perineal nerve (including the posterior scrotal nerves)35,36. Autonomic innervation of the prepuce arises from the pelvic plexus. The parasympathetic visceral efferent and afferent fibres arise from the sacral centre (S2-S4), and sympathetic preganglionic afferent and visceral afferent fibres from the thoracolumbar centre (T11-L2). The parasympathetic nerves run adjacent to and through the wall of the membranous urethra35. Although most neonatal and childhood circumcisions are performed with no anaesthesia37, the complicated innervation of the penis explains why a dorsal penile nerve block provides incomplete pain relief for neonatal male circumcision37,38. Likewise, a penile ring block cannot block the visceral afferent fibres from the cavernosal nerve nor the posterior scrotal somatosensory branches of the perineal nerve38. A eutectic mixture of local anaesthetic cream (EMLA) does not relieve the pain associated with circumcision because of the complexity of penile innervation and the multiple layers that would have to be penetrated by the topical cream in the newborn penis39. Amazingly, some modern urology textbooks even recommend wine as an anaesthetic for newborn circumcision24.
Researchers have documented that women with complete spinal cord injury may achieve orgasm with self-stimulation, suggesting that some sensory pathways of the genital tract may bypass the spinal cord by way of the vagus nerve40. Whether the external genitalia, including the prepuce, are innervated by the vagus nerve has yet tobe determined.
Although the sensory and autonomic innervation of the penis and clitoris are similar, there is a remarkable difference in their encapsulated somatosensory receptors. Sensory receptors can be classified as mechanoreceptors, e.g. Meissner's corpuscles (Fig. 4), Vater-Pacinian corpuscles (Fig. 5) and Merkel cells (Fig. 6); and nocioceptors (free nerve endings)41. A multitude of names have been used to describe these encapsulated receptors, e.g. Krause, Dogiel, genital corpuscles, Endkalpsen [sic] and mucocutaneous end-organs42, but the term corpuscular (encapsulated) receptors will be used here to include all of these mechanoreceptors. Most of the encapsulated receptors of the prepuce are Meissner corpuscles, as they contact the epithelial basement membrane.



The glans penis is primarily innervated by free nerve endings and has primarily protopathic sensitivity43. Protopathic sensitivity refers to cruder, poorly localized feelings (including pain, some temperature sensations and certain perceptions of mechanical contact)44. In the glans penis, encapsulated end-organs are sparse, and found mainly along the glans corona and the frenulum43. The only portion of the body with less fine-touch discrimination than the glans penis is the heel of the foot45. In contrast, the male prepuce ridged band (Fig. 7) at the mucocutaneous junction has a high concentration of encapsulated receptors46. The innervation difference between the protopathic sensitivity of the glans penis and the corpuscular receptor-rich ridged band of the prepuce is part of the normal complement of penile erogenous tissue.
In females, the glans clitoris and the inner plate of the prepuce have corpuscular receptors on their oppositional surfaces47. The glans clitoris also has a much denser concentration of Vater-Pacinian corpuscles than either the glans penis or the male prepuce. The fused common epithelium of the clitoris and the inner plate of the prepuce are reported to have intraepithelial nerves33. Merkel cells mediate tactile sensations, and are found in glabrous skin ; they have been reported in the clitoris and can be identified in the male prepuce (Fig. 6)49.
The mucosal epithelium of the male prepuce is the same as the squamous mucosal epithelium that covers the glans penis10. The glans penis and the inner prepuce share a common, fused mucosal epithelium at birth. Regardless of the embryological explanation, this common epithelium does not separate until the proper hormonal and growth factors are present. The epithelium of the clitoral prepuce is fused in the foetus and has intraepithelial nerves33. The fused inner plate of the male prepuce/glans has also been reported to have intraepithelial nerves50-52.
Ohmori50 described intraepithelial nerves within the common prepuce-glans penis epithelium in an 11.5-cm male embryo, but later studies by Winkelmann on newborn prepuces failed to identify intraepithelial nerves53. It is understandable why Winkelmann did not find these nerves, as he only studied amputated foreskins and not the normal, fused, prepuce/glans penile unit. Studies of the complete human foetal penis with careful attention to this area will be required before the assertions of Dogiel and Ohmori for intraepithelial nerves of the male prepuce can be dismissed. The mucosal epithelium also contains Langerhans cells, but does not contain melanocytes.
The lamina propria of the male and female prepuce is very vascular, which explains the common haemorrhagic complications associated with circumcision. The male prepuce has looser collagen than the dense collagenous lamina propria of the glans penis. The ridged band of the prepuce is near the mucocutaneous tip (acroposthion) of the male prepuce and, in the unretracted prepuce, usually lies against the glans penis46. The mucosal lamina propria (corion) is devoid of lanugo hair follicles, sweat and sebaceous glands46. Even in modern textbooks, Tyson's glands are often described as the source of smegma54; however, no evidence of Tyson's glands has ever been described outside of Cowper's macroscopic description of these glands in 169455. This may be one of the longest held myths in medicine55,56. Cowper's description of Tyson's glands in the human is actually of hirsutoid papillomas of the glans penis, which are fibroepithelial structures and not glandular structures55 Although other mammals have true clitoral and penile preputial glands which secrete sex pheromones, there is no current evidence of these glands inhumans57.
The dartos smooth muscle is specific to the male external genitalia and the vast majority of the penile dartos muscle is contained within the prepuce. The dartos muscle consists of smooth muscle cells invested with elastic fibres (Fig. 8). From the prepuce, the delicate, attenuated penile dartos muscle surrounds the shaft of the penis and is continuous with the scrotal dartos muscle. The penile dartos muscle is temperature-dependent and allows for the volume changes required for erection58. The function of the dartos muscle has been well described by Jefferson, and its loss to circumcision explains the altered response of the circumcised penis to temperature changes. In the infant, the muscle fibres are intertwined and arranged in a mosaic-like pattern59, causing the distal prepuce to pucker and close like a one-way valve60. When comparing the dartos muscle layer of the prepuce in males before and after puberty, the ratio of muscle fibres to elastic fibres decreases. This may explain why on gross inspection the distal prepuce is puckered in the infant and appears more relaxed in the adult. The increase in elastic fibres may be necessary for the uncomplicated eversion of the glans in the adult. While the aetiology of this transformation is unknown, steroid hormones may have an influence, as their topical application can accelerate the retractability of the prepuce in prepubescent boys61. Nerve bundles of the prepuce run alongside the dartos muscle.
The dermis of the prepuce consists of connective tissue, blood vessels, nerve trunks, Meissner corpuscles within the papillae, and scattered sebaceous glands. The dermis of the male prepuce appears to have more elastic fibres than the lamina propria of the prepuce. The difference between the elastic fibres in the preputial lamina propria and dermis may also help form the `muzzle' configuration around the glans penis. The elastic tissue of the prepuce dermis, along with the dartos muscle arid frenulum, tether the prepuce and help return it to its anatomically correct position after deployment during erection or after manual retraction.
The clitoral prepuce has only a dermal component with fewer elastic fibres than the male prepuce. The outer layer of the male and female prepuce has occasional sebaceous glands and sweat glands.
The outer epithelium of the prepuce consists of stratified squamous cells that are keratinized. Melanocytes are present in the basal layers. Langerhans cells and Merkel cells are also present (Fig. 6). The Langerhans cells are the first line of the body's immune defence system and are required for normal immune function. Merkel cells are specialized neuroendocrine cells that mediate tactile sensations and stain positively with cytokeratin 2010. The Merkel cells of glabrous skin contain characteristic membrane-bound dense core granules and are sometimes associated with unmyelinated neurites48. Merkel cells may express VIP, neurone-specific enolase, chromogranin A and cytokeratin 2010. The function and concentration of Merkel cells within the external genitalia has not been extensively studied.
The male preputial sac is moistened by secretions from the prostate, seminal vesicle and urethral glands of Littre56. Urine is not a normal component of subpreputial wetness56. The rich vascular plexus of the prepuce mucosa may facilitate production of a fluid transudate similar to that of the vaginal/vulva mucosa62. The female preputial sac is kept moist by a fluid transudate. Unlike some other mammals, the female preputial sac has not been shown to contain any preputial glands. VIP mediates the moistness of the aroused female genitalia62, but it is unknown whether it also contributes to the preputial moistness of the aroused male. The moist, lubricated male preputial sac provides for atraumatic vaginal intercourse.
The preputial sac is colonized by Cornybacterium, Gram-negative anaerobes (especially Bacteroides melamnogemcus), Enterococci, Enterobacteria and coagulase-positive Staphylococci63. Although Mycobacterium smegmatis is reported in a modern textbook as a possible factor in penile carcinogenesis64, attempts to show that M. smegmatis produces carcinogens or procarcinogens have been unsuccessful65,66. In the study by Neubert and Lentze53, acid-fast bacteria could be seen on the Ziehl-Nielsen smears, but nothing could be cultured in Lowenstein-Jensen medium. Therefore, the acid-fast organisms found in the preputial sac by Neubert and Lentze could have been mycobacterial contaminants from soil and water, such as M. gordonae67. Although M. smegmatis may be a commensal organism within the preputial sac it does not cause genital tract disease. However, M. smegmatis can cause non-genital soft-tissue infections after trauma or surgery68. The normal bacterial flora of the clitoral preputial sac has not been reported, but it would be assumed to be similar to the vulva, and would include Cornybacterium. Of interest, one study found M. smegmatis more commonly in female labial smears (46%) than in male urethral smears (4.5%)69. Furthermore, this study showed that circumcision had no effect on the recovery of acid-fast bacteria from the male urethra, and the presence of acid-fast bacteria did not cause urethritis. These data support the contention that M. smegmatis is a benign commensal organism within the external genital tract.
The preputial sac contains desquamated squamous epithelial cells similar to other mucosal cavities such as the oral cavity or vagina. This white, creamy material may collect under the prepuce of the clitoris (smegma clitoridis) or penis (smegma preputii). Male smegma has been shown to contain squalene, beta-cholestanol, sterols and long-chain fatty acids65,66,70. In men over 35 years old, 9,10-methyleneoctadecanoic acid is present, but it is not found in younger (17-20-year-old) males70. The function of the steroids, sterols and fatty acids produced within the human prepuce are unknown, but are considered to be protective elsewhere on the skin. In mammals that have preputial glands, sex pheromones and aggression-promoting pheromones are known to occur57,71.
Clinically, the presence of smegma preputii is a rare finding; in a prospective examination of 4521 uncircumcised boys, only 0.5% had smegma72. In adult men with clinically confirmed phimosis, only 6% had smegma present on examination73. Smegma can also be found in up to 25% of circumcised male children25 and can be detected in circumcised adults.
Although it has been known for many years that Langerhans and dendritic cells play an essential role in the cutaneous mucosal immune system, only recently has the mucosal immune system been used to prevented urinary tract infections by introducing antigens, i.e. immunisation, via the vaginal mucosa74. The immunologically active mucosal system of the prepuce may also provide a logical route of administering mucosal vaccines75.
Although it has been known that Langerhans cells can secrete cytokines76, only recently has it been discovered that squamous epithelial cells, with no Langerhans cells, can secrete cytokines and interleukin-1 that stimulate the immune response of T cells77. The cytokines released by the preputial mucosa and skin have not been carefully studied. Weiss et al. were unable to document Langerhans cells in the mucosal surface of newborn foreskins78, but in the adult prepuce, Langerhans cells are easily identified in the mucosal epithelium. The inability of Weiss et al. to find Langerhans cells in the newborn can be explained by the fusion of the preputial mucosa to the glanular mucosa in the sterile intrauterine environment. Langerhans cells would not be expected in the fused prepuce/glans penile mucosa until later in life, when the prepuce becomes retractable and the mucosa is exposed to antigens.
The role of the diversity of subpreputial flora in preventing infection has yet to be explored, as the study of the immunological function of the prepuce is in its infancy79. Circumcision has been justified by some because it removes the Langerhans' cells of the prepuce80 and therefore supposedly decreases the risk of HIV infections. This theory is flawed, as even after circumcision, there is residual penile mucosa of the glans, and there are Langerhans' cells in the penile shaft epidermis. Surgical removal of the Langerhans cells in all mucosa and skin to prevent infections is not feasible, nor rational. In addition, the aggressive circumcision campaign in the USA has not prevented sexually transmitted infections, including HIV. Therefore, Langerhans cells of the prepuce should be understood as normal mucosal immune cells, rather than a pathological entity requiring excision.
There is variability in the preputial coverage of the intact glans penis and clitoris. Some adult men have the glans penis completely covered by the prepuce while others have only partial coverage of the glans46,63. In a similar manner, the glans clitoris can be partially or completely covered by the prepuce; this merely represents anatomical variation.
The prepuce is primary, erogenous tissue necessary for normal sexual function8. The complex interaction between the protopathic sensitivity of the corpuscular receptor-deficient glans penis42 and the corpuscular receptor-rich ridged band of the male prepuce45 is required for normal copulatory behaviour. The increased frequency of masturbation, anal intercourse and fellatio reported by circumcised men in the USA81 may possibly be due to the sensory imbalance caused by circumcision. Clearly, amputation of the prepuce causes changes in sexual behaviour in human males81 and females82.
Surgical amputation of the prepuce removes many of the fine-touch corpuscular receptors from the penis and clitoris. In males, circumcision is essentially a partial penile mucosectomy. The residual exposed glans mucosa becomes abnormally keratinized with an increase in the number of cell layers in glanular mucosal epithelium. The urethral meatus is exposed and prone to irritation. Meatal stenosis can be a complication after circumcision. During circumcision, the frenular artery may also be ablated, depriving the anterior urethra of its major blood supply. The combined effect of urethral ischaemia and irritation results in the development of meatal stenosis in 5-10% of circumcised males25,83,86. The risk of glanular injury when tearing the fused penile mucosa, and the development of meatal stenosis, makes circumcision in the newborn period inadvisable87-89.
During circumcision, most of the penile dartos muscle is removed; all that remains is a few bundles of muscle at the circumcision scar. It has been observed that the flaccid penis in circumcised males tends to hang less vertically than in those with complete anatomy. The loss of dartos muscle support may explain the difference. Certainly, the loss of most of the penile dartos muscle makes the penis less able to make positional adjustments during erection and with temperature changes.
For unknown reasons, keloid formation after circumcision is quite rare90,91. Although the circumcision scar has not been thoroughly studied, there are several different theories as to what happens when the nerves of the sensory receptors of the prepuce are transected during circumcision. Some have speculated that after circumcision, these nerves regenerate and develop new encapsulated receptors92. According to this theory, there would be a significant loss of penile sensitivity after circumcision, but this loss would not be apparent 6 months after the circumcision92. This notion is in direct conflict with human and animal studies that show when a nerve is transected, and the distal tissue is amputated, the proximal nerve undergoes acute axonal swelling93-95. After acute injury, the axon begins to sprout and branch at the injury site. Without the distal nerve, this frustrated attempt at re-innervation results in a bulbous, disordered tangle of axons, Schwann cells and fibrous tissue. Histology of the male circumcision scar shows amputation neuromas, Schwann cell proliferation and the bulbous collection of variably sized neurites. Amputation neuromas do not mediate normal sensation and are notorious for generating pain. Animal studies show that extirpation of the external genitalia results in acute retrograde degeneration of the nerve axon back to the spinal cord96. Therefore, the changes in circumcised male sexual behaviour81 may be related to a central nervous system alteration by retrograde axonal degeneration, or to peripheral nervous system damage by loss of the prepuce ridged band and amputation neuroma. It is assumed that amputation neuromas also form at the female circumcision scar, although we are unaware of a formal histology study.
Although foreskin restoration cannot regenerate dartos muscle or encapsulated sensory receptors, it appears that the residual stump of prepuce could be stretched to provide partial covering of the coronal sulcus and corona. This re-covering of the corona, combined with a reversion of the epithelium to the normal squamous mucosa of the glans, may account for the improved sensitivity reported by men who have nonsurgically restored their foreskins97. Likewise, it appears that restoration of the female vulva after circumcision may provide subjective improvements in sensitivity and selfesteem98. Further histological examination and somatosensory evaluation of the circumcision scar and the restored foreskin is needed to explain the altered sensitivity reported by circumcision and restoration.
The prepuce is a specialized, specific erogenous tissue in both males and females. Therefore, surgical excision should be restricted to lesions that are unresponsive to medical therapy, such as lichen sclerosis of the penis (balanitis xerotica obliterans) or vulva, which is unresponsive to other therapies (e.g. topical clobetasol, intralesional corticosteroids, topical testosterone propionate ointment, etretinate, and carbon dioxide or laser vaporization)99. Preputial plasty100 should be considered in place of circumcision whenever possible, so as to preserve the corpuscular sensory receptors, dartos muscle, penile mucosa and complete function of the penis, while avoiding abnormal exposure and keratinization of the glans penis. Although some cultures celebrate the abnormal anatomy caused by circumcision, many women101,102 and men103 have reported this abnormal penile/clitoral exposure to be uncomfortable. The male prepuce contains the vast majority of the penile dartos muscle that cannot be regenerated after circumcision. The preputial mucosa and outer epithelium provides adequate epithelial coverage of the erect penis.
The loss of the prepuce ridged band and the formation of an amputation neuroma are two further complications associated with male circumcision. Although a Fourcroy grade 1 female circumcision would excise less tissue than in a male, this comparison cannot be used to justify female circumcision. Excision of normal, erogenous genital tissue from healthy male or female children cannot be condoned, as the histology confirms that the external genitalia are specialized sensory tissues.
The complex anatomy and function of the prepuce, along with the fused prepuce/glans penile mucosa in the immature penis, dictates that neonatal circumcision be strictly avoided, as recommended by the Australasian Paediatric surgeons88, Canadian Paediatric Society89, and a paediatric urology textbook87. Removal of normal genital anatomy in children and infants should be deferred until the individual can make an informed decision104. If external genital tissue must be excised to combat a disease process that threatens the child's health, and is unresponsive to medical therapy., then the amount of tissue should be limited so as to preserve the anatomy and function of the external genitalia. All genital tissue excised from children should be microscopically examined to confirm the clinical opinion of the disease. As physicians and parents learn the normal anatomy and functions of the external genitalia, there will be greater understanding of its essential nature, and more attempts to limit its removal.
We thank Drs. Michelle Storms and Ken McGrath for invaluable editorial assistance; Barb Bartkowiak, Alana Ziaya. Tracey Heldt and Joann Gumz for library assistance; Marshfield Clinic graphic arts, and the histology section of pathology for their expertise and help: Steve Booher for photographs; Shirley Thompson for drawings; Laura Bliven forimmunoperoxidase staining.
Love Surgery. American Medical News 1989; Jan 27; 1-12
C.J. Cold, MD, Pathologist.
J.R. Taylor, MB, ChB, MRCPED, FRCPC, Pathologist.
Correspondence: Christopher J. Cold, MD, Department of Pathology, 1000 North Oak Ave, Marshfield, Wisconsin, 54449, USA.
E-mail: coldc@dgabby.mfldclin.edu
The Circumcision Information and Resource Pages are a not-for-profit educational resource and library. IntactiWiki hosts this website but is not responsible for the content of this site. CIRP makes documents available without charge, for informational purposes only. The contents of this site are not intended to replace the professional medical or legal advice of a licensed practitioner.
© CIRP.org 1996-2026 | Filetree | Please visit our sponsor and host:
IntactiWiki.